I'm sure you're thinking, what does a UTI have to do with constipation? We get it, one is from the front, and one is from the back. But guess what? The two conditions actually have a lot to do with each other. In fact, what you think is a UTI might just be symptoms of constipation. Sounds odd, but the two parts are actually intertwined. We'll explain.
Constipation occurs when stool remains in the colon for too long or moves too slowly through the colon. As the poop remains in the colon, fluid is reabsorbed by the body. The longer the stool remains, the accumulation of stool puts pressure on the bladder. In addition, the more poop that is backed up can make the colon expand, adding even more pressure on the bladder, which causes either increased spasm or outflow obstruction. The bladder, which stores urine, is located near the rectum. Make sense?
The lower belly pressure is often associated with symptoms of a UTI. Plus, the physical pressure of the poop also constricts the urethra, making it difficult for the body to hold urine, leading to urinary urgency. Another symptom of a UTI. When constipation and frequent urination occur at the same time, it can be bladder and bowel dysfunction (BBD). This condition is not a bacterial infection like a UTI, so no antibiotics are needed.
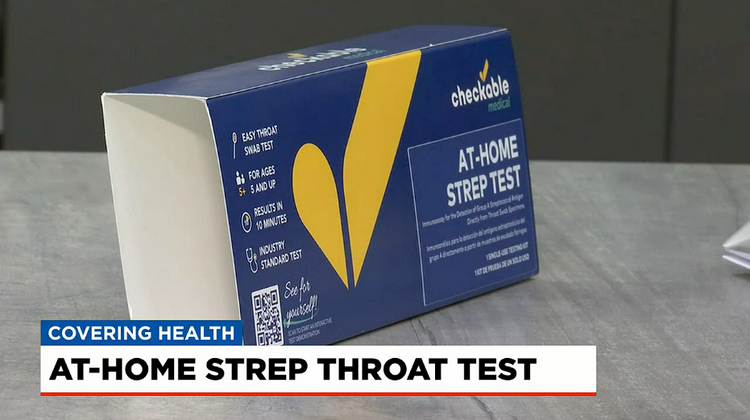
So, how do you know if it is a UTI or just backed up? Well, the only true way to tell is to take an at-home (or at your dr. 's office) UTI test, but it is also a good idea to first evaluate your symptoms. If you feel the pressure and urgency to pee but no pain while peeing, and you notice you haven't pooped in over three days, there is a good chance that you may need to bulk up on fiber!
Chronic Constipation and UTIs
Aside from constipation bringing on similar symptoms of UTI pain, there is also a higher chance of getting recurring UTIs in those who also suffer from chronic constipation. Especially in children and post-menopausal women. Sigh. Like the bloat isn't enough. The relationship between the two also stems from the fact that the colon and rectum are right behind the bladder. If your colon is full and presses on your bladder walls, a few things can cause UTIs.
- Bladder Obstruction: As stool accumulates, the waste of the colon and rectum expands and starts pressing on the bladder. This congestion might prevent you from completely emptying your bladder when you pee. The longer the pee sits in the bladder, the greater the chance bacteria will grow and cause a UTI.
- Backward Urine Flow: The pressure from the colon can also cause the urine to flow backward from the urethra to the bladder, lifting any bacteria which might have been in your urethra up to the bladder and causing a UTI.
- Disrupted Flora: Chronic constipation can lead to high levels of the Escherichia coli (E. coli) bacteria in the rectum, increasing the risk of it spreading to the urinary tract. Probiotics can help with this. Laxatives can be a culprit, so opt for bulk-forming fiber intakes like Metamucil or Citrucel.
- Overactive Pelvic Floor: All the straining from constipation can lead to overactive pelvic floor muscles that can contribute to recurrent UTIs as well. This can result in the dysfunctional elimination of stool and urine and actually cause bladder overactivity or bowel dysfunction. The storing of waste and old urine can cause bacteria to grow and cause a UTI.
What’s the takeaway here? Well, the bottom line is if you notice that you go number two less than three times a week, there is a chance that you can be a candidate for chronic UTIs. Or, you may actually not even have a UTI at all but instead, just be really constipated. Treating constipation should help with both. Increase fiber intake, avoid laxatives, take probiotics for the gut and bladder, exercise, and always practice good hygiene!
Life is too short to sit in a doctor’s office
Sign up for our weekly newsletter and get valuable healthcare tips and tricks in your inbox!
Sign up now and unsubscribe anytime.
- Choosing a selection results in a full page refresh.
- Press the space key then arrow keys to make a selection.